Head and neck cancers encompass a diverse group of malignancies affecting areas such as the oral cavity, pharynx, larynx, nasal cavity, and salivary glands. Treatment often involves surgical resection, which can lead to significant defects impacting essential functions like speech, swallowing, and appearance. In such cases, reconstructive surgery becomes vital to restore both aesthetics and function.
One of the most advanced techniques in reconstructive surgery is free flap reconstruction. It involves transplanting tissue from one part of the body to another to repair complex defects. Dr. Leena Jain, a prominent plastic surgeon in Bandra, Mumbai, emphasizes, “Free flap reconstruction has revolutionized the way we approach complex head and neck defects, offering patients a chance at a better quality of life post-surgery.”
Being a seasoned plastic and reconstructive microsurgeon, Dr. Jain specializes in hand surgery, tumor and trauma reconstruction, and breast surgery. Known for her patient-centered care and surgical excellence in head and neck cancer reconstruction, she employs cutting-edge free flap techniques to achieve excellent functional and aesthetic outcomes.
What is a Fibroadenoma?
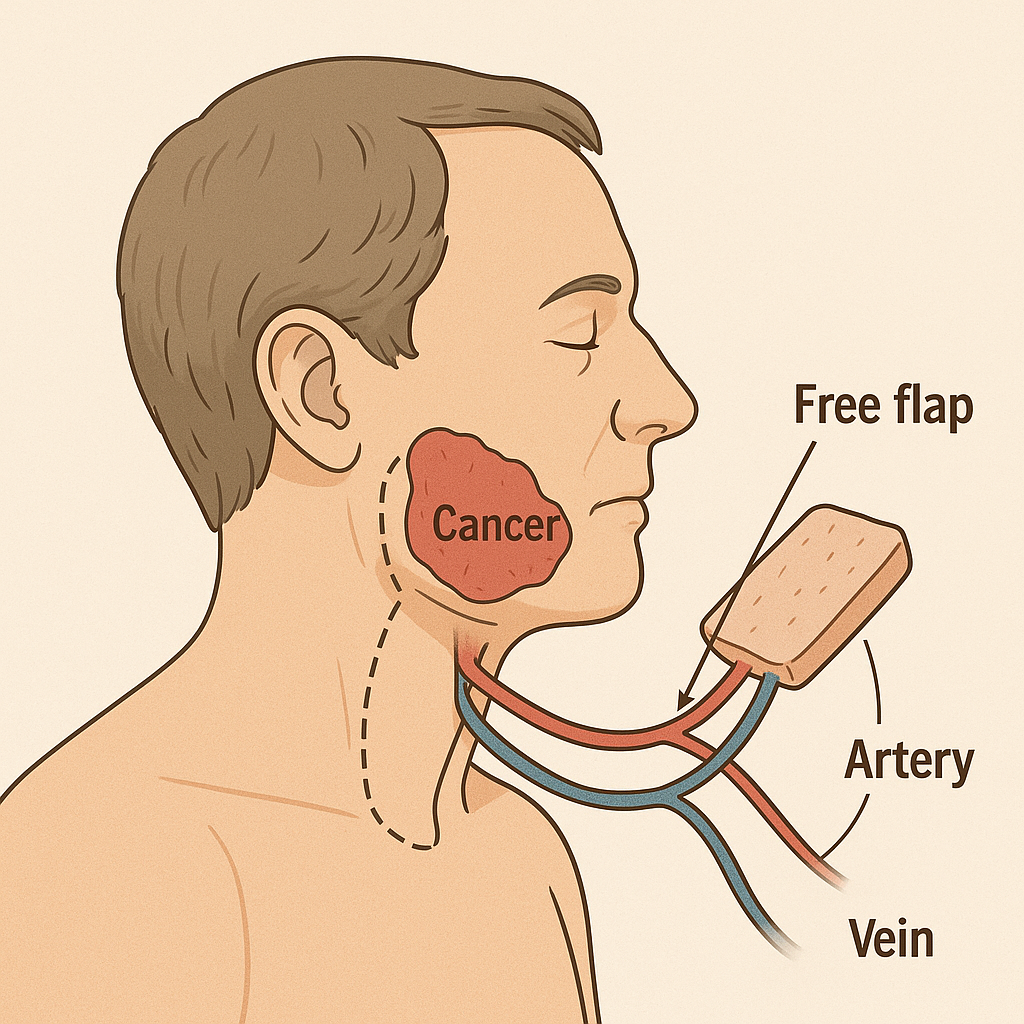
Free flap reconstruction, also known as microvascular free tissue transfer, involves transplanting tissue, comprising skin, muscle, fat, or bone, from a donor site to a recipient site, reconnecting blood vessels using microsurgical techniques. This method ensures the transplanted tissue remains viable, promoting healing and functionality.
Unlike pedicled flaps, which remain attached to their original blood supply, free flaps are entirely detached and reconnected at the new site, offering greater flexibility in reconstructing complex defects.

Restore form and function with expert guidance. Connect with a skilled specialist for a personalized evaluation and explore your options!
The Critical Role of Free Flap Reconstruction in Head and Neck Cancer
In head and neck cancer surgeries, especially those involving extensive tissue removal, free flap reconstruction plays a pivotal role in restoring essential functions and aesthetics. By using tissue from other body parts, surgeons can reconstruct areas affected by cancer resection, aiding in speech, swallowing, and appearance.
This technique has become the standard of care for many complex head and neck defects, particularly after oncological resections. It allows for tailored reconstruction, addressing patients’ functional and cosmetic needs.
Common Types of Free Flaps Used
A variety of free flaps are used depending on the nature of the reconstruction:
-
Radial Forearm Free Flap (RFFF):
Ideal for soft tissue reconstruction due to its thin and pliable nature.
-
Anterolateral Thigh (ALT) Flap:
Offers a large volume of tissue, suitable for extensive defects.
-
Fibula Free Flap:
In mandible reconstruction, used mainly to provide both bone and tissue.
-
Scapular and Parascapular Flaps:
They provide versatile tissue options with low donor site morbidity.
“The choice of flap depends on factors such as defect size, location, and the patient’s general health,” explains Dr. Leena Jain, a well-known plastic surgeon in Mumbai.
How the Procedure is Performed
The free flap reconstruction procedure involves several meticulous steps:
1. Donor Site Preparation:
The surgeon harvests tissue from the donor site, ensuring minimal impact on function and appearance.
2. Recipient Site Preparation:
The area requiring reconstruction is prepared, and recipient blood vessels are identified.
3. Microsurgical Anastomosis:
Using a microscope, the surgeon connects the arteries and veins of the flap to those at the recipient site, restoring blood flow.
4. Flap Inset and Monitoring:
The flap is shaped and secured into place, with continuous monitoring to ensure viability.
This intricate procedure demands high surgical expertise and precision to ensure successful outcomes.
Benefits and Challenges of Free Flap Reconstruction in Head and Neck Cancer
Benefits:
- Functional Restoration:Improves speech, swallowing, and breathing.
- Aesthetic Improvement:Enhances appearance, boosting self-esteem.
- Versatility:Allows for reconstruction of various tissue types and sizes.
Challenges:
- Complexity:Demands sophisticated surgical technique and instrumentation.
- Risk of Complications: Flap failure or infection risk.
- Extended Recovery:Longer healing period than other procedures.
Though there are challenges, the advantages usually exceed the risks, giving patients a chance at better quality of life.
Recovery and Postoperative Care
Postoperative care is the key to successful free flap reconstruction:
-
Monitoring:
Periodic checks to maintain flap viability and identify complications early.
-
Wound Care:
Cleanliness and dressing of donor and recipient sites.
-
Rehabilitation:
Speech and swallowing therapy might be required.
-
Follow-Up:
Frequent visits to track healing and address any queries.
Compliance with postoperative instructions improves recovery and overall results.
Conclusion
FAQs
Why is free flap reconstruction significant in head and neck cancer?
What components of the body can be harvested for free flap donor tissue?
How long is recovery following free flap reconstruction?
Are there complications of this surgery?
Will there be noticeable scarring?
What’s the difference between a free flap and a local flap?
How do I look after the donor and recipient sites post-operatively?
Follow your surgeon’s post-operative care advice strictly. Wound care, monitoring signs of infection, and avoiding strain are essential.
Reference links:
https://link.springer.com/book/10.1007/978-3-030-29582-0
https://pmc.ncbi.nlm.nih.gov/articles/PMC8329401/
Disclaimer: This page is for informational purposes and not for promotional use.